Watching Brief
Increase in cases of Diphtheria in Europe among asylum-seekers
| Date of first report of the outbreak | 14 June 2022 |
| Disease or outbreak | Diphtheria |
| Origin (country, city, region) | Austria, Europe |
| Suspected Source (specify food source, zoonotic or human origin or other) | Human to human transmission |
| Date of outbreak beginning | 1 June 2022 |
| Date outbreak declared over | 26 September 2022 |
| Affected countries & regions | Seven European nations - Austria, Germany, Norway, Belgium, France, Switzerland, United Kingdom |
| Number of cases (specify at what date if ongoing) | Of the 144 cases, 97 were classified as clinically compatible, 44 were laboratory confirmed as toxigenic diphtheria cases and three were suspected cases all between June and September 2022 (1). |
| Clinical features | Diphtheria is a severe infection that affects the upper respiratory tract, leading to pseudo-membrane formation, neck swelling, and suffocation. It can also cause cutaneous infections (2). Diphtheria toxin production by Corynebacterium diphtheriae can cause damage to the heart and other organs. Non-toxigenic strains can also cause invasive infections (3). Of the 44 cases, 43 were caused by C. diphtheriae and one by C. pseudotuberculosis, with cutaneous diphtheria in 35 cases, mild/asymptomatic in eight cases and classic respiratory diphtheria in one case that resulted in death (1). |
| Mode of transmission (dominant mode and other documented modes) | Diphtheria is transmitted by direct contact or by sneezing or coughing (4). The dominant mode of transmission occurs by exposure to droplets during close contact with an infected person or by contact with carriers of the Diphtheria strain, more rarely with contaminated objects or direct contact (4). Diphtheria also spreads through infected animals, unpasteurized milk and contaminated food (5). |
| Demographics of cases | Of the 144 cases in this outbreak, 90 cases were reported among asylum seekers or refugees, primarily from Afghanistan (52 cases) (1). 32 cases were local European residents, three of whom were reportedly infected abroad (1). For 22 reported cases, the affected population was not reported. Gender was known in 71 cases, of which 67 cases were males and four cases were females (1). Two diphtheria outbreaks in a Swiss asylum center were reported from July to September 2022 (6) |
| Case fatality rate | In the current outbreak, the case fatality rate is less than 1%. Classic respiratory diphtheria that occurred in one case resulted in death (1). Diphtheria is a serious disease with 5%–10% of all people with diphtheria ending in death. Up to 20% of cases lead to death in children younger than age 5 years and adults older than age 40 years (7). The mortality rate from pharyngeal diphtheria is high and can reach 50% (7). |
| Complications | After an infection, the skin, lungs, heart, nervous system and kidneys can be damaged. A diphtheria infection can lead to myocarditis, peripheral neuropathy, pneumonia or respiratory failure (8, 9) |
| Available prevention | Vaccination protects against the disease. It should be given to children between the ages of two, four and 12 months, and between four to seven and 11 to 15 years. Additional booster vaccinations are recommended at age 25, 45 and 65 and then every 10 years. Countries like Austria, Norway, Belgium, France and Germany all follow a similar vaccination schedule in their national immunization strategy (10). Switzerland also follows this recommended vaccination schedule (11). |
| Available treatment | The disease can be treated with an antidote and antibiotics (12). Equine diphtheria antitoxin (DAT) in combination with antibiotic treatment (penicillin) or a macrolide (erythromycin, azithromycin or clarithromycin) is prescribed for a period of 14 days (13). |
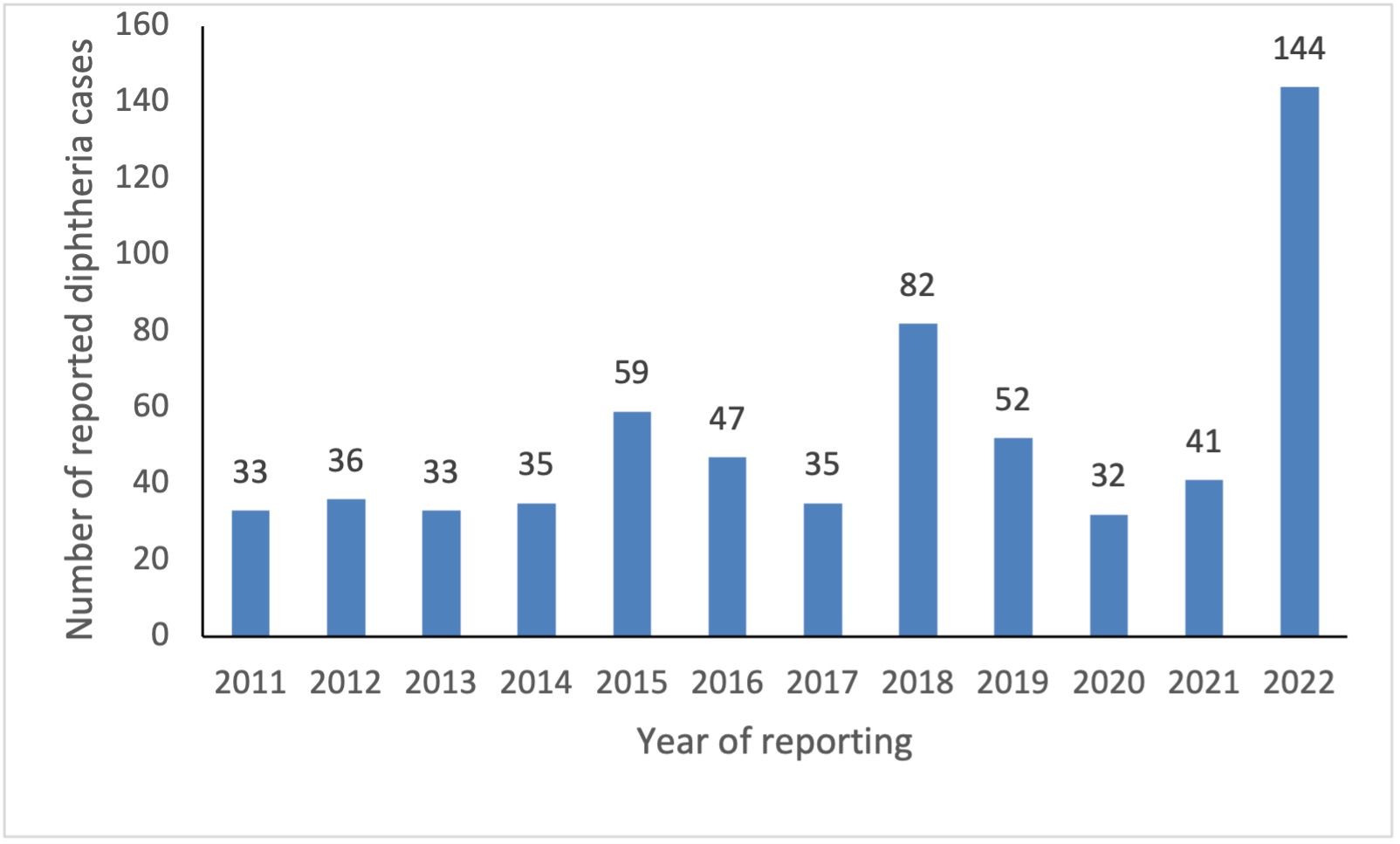
| Comparison with past outbreaks | Diphtheria is a rare disease in Europe. An average of 52 cases were annually reported across Europe to European Centre for Disease prevention and Control (ECDC) between 2016 and 2020. Around 50% of reported cases were caused by Corynebacterium diphtheriae. Of the 128 cases caused by C. diphtheriae reported between 2016-2020, 60 were cutaneous, 25 respiratory, and one had both a cutaneous and respiratory presentation. During this five year period, 69 C. diphtheriae cases were classified as imported and of these, 46 presented with a cutaneous disease (1). It was not possible to confirm the potential migratory status of these cases as their reason for travel to the Europe was not reported (14).
Figure 1
Distribution of reported Diphtheria cases by year in the Europe region, 2011-2022 (1) The recent increase in the number of cases reported, seen in Figure 1, could be explained by an increased volume of migrants from diphtheria-endemic countries, by an increased circulation of the pathogen in the countries of origin, or an increased risk of transmission in specific settings such as migrant reception centres. As of 26 September 2022, ECDC is not aware of any evidence indicating outbreaks in the broader European population resulting from the increased number of imported cases (1). Hence, migration is said to be the most important factor contributing to the most recent outbreak, and asylum seekers and immigrants were mostly affected. |
| Unusual features | Epidemiological transition The diphtheria cases that occurred in this outbreak are mostly among adults rather than children. In the pre-vaccine era, exposure to toxigenic strains of diphtheria organisms was common, children were susceptible, and most adults remained immune to the disease. However, after immunization of children became widespread, diphtheria became rare, so exposure to these bacteria (and the concomitant natural boost of immunity) became uncommon. If adults do not have natural exposure to diphtheria-causing organisms or receive booster doses of diphtheria toxoid, their immunity induced by childhood immunization wanes, and they become susceptible to the disease (15). This is known as epidemiological transition. From 2011 to 2019, most diphtheria cases were reported in adults aged 30 years and older. This finding concurs with that reported in recent reviews of diphtheria epidemiology that showed an age distribution shift, with cases mostly occurring in adolescents and adults (16, 17). These changes in the age-wise distribution of the immunity patterns usually have been explained by the argument that immunization led to a marked decrease in the incidence of the disease and to a subsequent reduction of the reservoir of toxigenic C. diphtheriae organisms (15). Low fatality rate Early detection through surveillance and opt treatment with antibiotics and DAT was mainly responsible for the reduction in the mortality among the infected in this outbreak (6). Lack of spread in local populace Of the 144 cases, 90 (63%) were asylum seekers or refugees, while 32 cases (23%) were local residents, three of whom were reportedly infected abroad. Although immigrants and asylum seekers are the majority among the infected, there is not much spread in the local European population (1). This could be attributed to the increased vaccination coverage among the European populations when compared with immigrants (18). |
| Critical analysis | The major reasons that could attribute to the increase in number of imported cases in Europe could be as follows. Sudden influx of immigrants post Covid19 lockdown Due to the travel restrictions and border closures, imposed by governments globally, several migrants – including seasonal workers and international students – were stranded and unable to return to their countries of origin (19). Also, the asylum seekers were not able to cross borders until the restrictions were lifted. Once the lockdown was relaxed, there was a sudden increase of migrant and asylum seekers into Europe, resulting in an increase in infection rate (20). This shows that the number of cases reported so far in 2022 is higher than the average number of imported cases seen in recent years (1). Lack of herd immunity in migrants Long term protection against diphtheria has been shown to be insufficient among migrant populations (21).This might be due to lack of herd immunity in the migrant population, as evident in previous studies. Vaccination coverage imbalance among European and low-income nations Due to the Covid19 lockdown, the vaccination coverage for all vaccine preventable diseases had seen a dip worldwide, especially in countries like Afghanistan, which has been war torn for several decades (22). Hence asylum seekers from such countries are easily suspectable for vaccine preventable diseases like diphtheria. The relatively low number of cases reported annually in recent years in Europe is probably the result of overall long-standing high vaccine coverage at regional level (14, 23). For 2012–2021, based on World Health Organisation (WHO) / United Nations International Children’s Emergency Fund (UNICEF ) Estimates of National Immunization Coverage, coverage in Europe with the first dose of diphtheria, tetanus, pertussis vaccine (DTP1) and the third dose of diphtheria, tetanus and pertussis vaccine (DTP3) was 95–97% and 92–96%, respectively (18, 24, 25) This imbalance in vaccination coverage results in difference in infection rate among migrants and European people. Genetic diversity of isolates of various strains of Diphtheria The genetic diversity of isolates are indicative of multiple spreading events among asylum seekers. Multiple spreading events are due to different routes of travel by asylum seekers (6). Challenges to treatment due to anti-microbial resistance Anti-microbial resistance to penicillin and macrolides, which are usually the first line of drugs against diphtheria, poses a challenge in reducing the mortality and morbidity in affected cases. In such cases multi-drug regimen is opted for treatment (26). This also results in partially treated or asymptomatic carriers that spread the disease at an increased rate. Surveillance for Diphtheria cases in Europe For 2012–2021, 452 diphtheria cases were reported in Europe through the UNICEF Joint Reporting Form (JRF) submitted by each country to the WHO (14, 23). From the period 1 January to 31 August 2022, 144 diphtheria cases detected in the region were reported to the WHO through the IHR system (23). Most of the cases were detected in the summer months of June through August (27). Thus, the WHO is effectively able to maintain a reporting system for vaccine preventable diseases. |
| Key questions | 1. How to improve screening and surveillance for vaccine preventable diseases especially for Diphtheria in asylum seekers and immigrants in Europe? These key questions result in the following recommendations: |
| Acknowledgements | This Watching Brief is an output of an epidemiology workshop between The National Institute of Epidemiology and EPIWATCH |