The 2014-2016 West African Ebola Virus Disease epidemic (caused by Ebola Zaire strain; hereafter referred to as EVD) was one of the worst outbreaks of the 21st century. Never before had EVD spread so aggressively over such a vast geographical area [1], as historically the virus usually appeared in remote areas throughout the central African equatorial forest block [2]. The index case originated from a Guinean village following the death of a young child exhibiting typical symptoms associated with viral haemorrhagic fevers in December 2013 [3]. By July 2014, the virus had spread to Liberia and Sierra Leone [4], being transmitted at an unprecedented rate. From the initial cases recorded between December 2013 and September 2014, 4,507 confirmed/probable cases were reported to the World Health Organisation (WHO) [5]. By the end of the outbreak, over 11,000 people died as a direct consequence of EVD, although this figure does not take into consideration the additional death toll associated with the wider disruption caused by the virus [1].
Many suggestions have been put forward in explaining why the virus spread so aggressively, especially compared to previously more contained outbreaks. Médécins Sans Frontières (MSF) argued that passivity and the reluctance to act both within and outside the West African context provided time for complex chains of transmission to develop [1]. Others highlighted the key role cultural practices, poor health infrastructure and political corruption had in spreading EVD [6, 7]. Although an account of all the factors involved is beyond the scope of this review, we focused on one particular aspect of the outbreak, namely the interconnection between beliefs and/or practices and control measures used (such as health promotion or safe burial initiatives). More specifically, the focus was on the wider effects that cultural, biological, ecological, and political forces had in terms of influencing engagement with disease control. Taking such a holistic approach ensured that wider ecological factors (such as resources and political corruption) were not belittled at the expense of more common and clichéd explanations (i.e. overemphasising the role cultural traditions had in spreading EVD) [8].
In investigating such an interconnection, it is important to outline a key theoretical paradigm which played a critical role in interpreting our findings. Building from the wider ‘ecological’ wave in public health promotion [9], we decided to adopt Barry Hewlett’s Evolutionary Cultural Anthropology (ECA) approach, which centres on the interconnectivity between social and cultural factors that shape EVD outbreaks [10]. ECA itself consists of a few different components, which include cultural considerations (burial practices), culturally constructed niches (gendered caring roles), ecological factors (proximity to bush-meat) and human biology/nature (fear) [10]. Being a triangulated framework, each component has an interactive role which affects the other factors, ultimately shaping behaviour.
More recently, such anthropological frameworks, which tend to frame human behaviour through socio-cultural paradigms, have been acknowledged as having a crucial role in global health emergencies [11]. Having said that, Hewlett’s theoretical framework was specifically chosen due to its compatibility with the conceptual orientation of this project, as his previous work underpinned the very design of this review [12]. Accordingly, we decided to investigate how his most recent theoretical contribution (ECA) could be used in interpreting findings from empirical work conducted throughout the West African EVD outbreak – an approach which has not yet been pursued. Consequently, in terms of implications for this review, we sought to answer two critical questions. First, what role did certain beliefs and/or practices, held by the general public in Sierra Leone, Liberia, and Guinea, play in either hindering or promoting disease control during the outbreak? Second, building from our findings, if required how could Hewlett’s framework be improved?
Although some reviews have touched on similar themes, especially in terms of EVD and qualitative research more broadly [13-15], to the best of our knowledge no qualitative synthesis, which specifically provides both theoretical and practical insights into disease control dynamics observed during the West African EVD outbreak, currently exists. Therefore, we aimed to address this gap by adopting a qualitative evidence synthesis method in relation to answering the two abovementioned critical research questions.
Authors TB and NRC were involved in the review design, which was developed based on guidance set out by both Cochrane and Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) [16] (supplementary file 1). Additionally, inclusion and exclusion criteria were devised via a Population, Interest and Context (PICo) protocol (supplementary file 2) [17]. In terms of our research questions, such a protocol was more suitable for the qualitative orientation of our review, compared to more quantitative protocols [18]. The population and context in our review consisted of people living (the general public) in West Africa during the outbreak. The interest was thematically identifying which beliefs and/or practices either hindered or promoted disease control.
Importantly, we only focused on countries which experienced widespread transmission during the outbreak (Liberia, Guinea and Sierra Leone) – as determined by the Centres of Disease Control and Prevention (CDC) in terms of suspected, probable and confirmed infection rates [4]. Furthermore, only published peer-reviewed articles written in English and conducted during or after the outbreak from the perspective of the general public were included. We adopted the CDC timeline beginning in 2014, which coincides with the formal outbreak declaration set out by the WHO on 23rd March 2014 [4]. Table 1 outlines all inclusion/exclusion criteria used within this review. It should also be noted that due to time constraints, this review was not registered via the International Prospective Register of Systematic Reviews (PROSPERO) in health and social care. As such, there is no initial published protocol for this review. However, we followed established protocol as outlined by Cochrane and PRISMA guidance as well as qualitative-specific systematic review guidance [17].
Table 1
Inclusion and exclusion criteria used in this review
| Criteria: | Justification: |
| 1)The publication must be in English. | Due to the size of the review team, we do not have the resources to translate papers. |
| 2) The paper must contain primary or secondary research. | As this review is centered on the experiences of those who lived through the West African outbreak, only publications that involve primary/secondary research can be used in answering the set research questions. |
| 3)The research must have been conducted during or after the outbreak within west African countries that experienced widespread EVD transmission. | Including research outside of this parameter would undermine the PICo framework, and thus would be irrelevant in answering our research questions. Further, this parameter was set based on the CDC and WHO timeline of events. Therefore, data collection had to begin after 1st January 2014, and had to have been conducted in either Sierra Leone, Guinea or Liberia. |
| 4) A qualitative approach to data collection/analysis must have been used. | This is a qualitative systematic review, so any research that only included quantitative methods cannot be included. However, mixed method studies were included. |
| 5) The sample must include people from the general population and not just healthcare workers. | This review is focused on the experiences of the general public during the outbreak. Thus, ideal studies for this review would include a sample primarily including members of the general public. However, exceptions can be made for ambiguous community centered roles (i.e., community liaison officers). Some studies however only focused on the views of healthcare workers - these were excluded. Unless otherwise stated, primary quotes (constructs) used in the synthesis are from members of the general public and not healthcare professionals. |
| 6) Full text Portable Document Format (pdf) of the study had to be available. | If the publication could not be accessed either through Google Scholar or the University of Glasgow's library service, it was excluded. |
| 7) Must be a published journal article. | Due to the size of the review team and time constraints, it would not be feasible to synthesise all white and grey literature. Therefore, only published peer-reviewed papers were included. |
Database selection and search strategy development was an iterative process. Rather than adopting purposive sampling techniques, a comprehensive approach was taken [19]. Originally, five electronic databases were searched from May to June 2021. These included Medline (Ovid), Embase (Ovid), PubMed, Scopus and Cumulative Index of Nursing and Allied Health Literature (CINAHL). Table 2 outlines the search strategy used within the latter databases (see supplementary file 3 for a more extensive list). Minor variations were made where controlled vocabulary could not be utilised (i.e., Scopus). During the analysis and write up of the synthesis, the databases were searched again (February 2022) to ensure our work was as up to date as possible. This also included hand/citation searching which was continually conducted up until April 2022.
Table 2
Search strategy used (example from Medline)
| N. | Search line |
| 1 | Hemorrhagic Fever, Ebola/ |
| 2 | (ebola or ebolavirus).ti,ab. |
| 3 | 1 OR 2 |
| 4 | exp Health Promotion/ or exp Health Behavior/ or exp Communicable Disease Control/ or exp Community Participation/ |
| 5 | (Health Promot* or Health Behavior* or Health Behaviour* or Disease Control* or Community Engagement).ti,ab. |
| 6 | 4 OR 5 |
| 7 | exp Culture/ or exp Health Knowledge, Attitudes, Practice/ or exp Attitude to Health/ or exp Anthropology, Cultural/ |
| 8 | (Cultur* or Health Knowledge or Attitud* or Perceptio* or Belief or Beliefs or Denial* or Denying or Deny).ti,ab. |
| 9 | 7 OR 8 |
| 10 | exp Qualitative Research/ |
| 11 | (focus group* or interview* or participant observation* or case stud* or survey* or questionnaire* or secondary analy* or secondary research or ethnograph*).ti,ab. |
| 12 | 10 OR 11 |
| 13 | 3 AND 6 AND 9 AND 12 |
The screening process involved both abstract and full text screening. Authors TB and VW were involved in the double-blind abstract screening process, after which a consensus meeting (mediated by NRC) was held to discuss any disagreement. Between TB and VW, there were no major disagreements between included/excluded studies. Following this, TB conducted full text screening. Included studies were then checked for quality by TB using a variation of the Critical Appraisal Skills Programme (CASP) checklist (supplementary file 4). After critical appraisal, both study characteristics and data (first and second order participant/author constructs) were thematically extracted (supplementary file 5) by TB, after which thematic analysis and synthesis was conducted with NVivo 12 in line with the protocol set out by Thomas and Hardon [20].
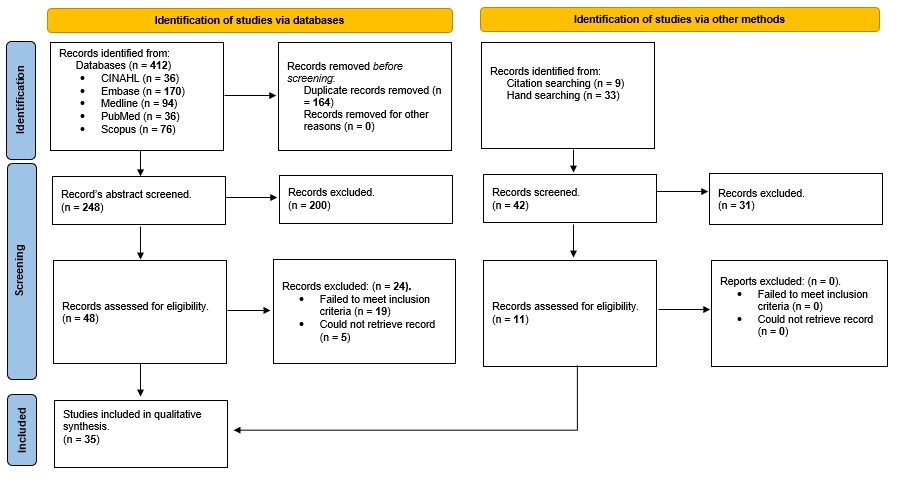
Overall, 35 studies were included, with 24 obtained via systematic searching and 11 through hand/citation searching (Figure 1). Excluded papers failed to pass either our abstract (n=231) or secondary (n=24) screening criteria. For instance, some papers did not include a sample which involved members of the general public. Additionally, others could not be accessed electronically and were therefore excluded (supplementary file 6).
Results of systematic searching, PRISMA 2020 flow diagram for systematic reviews [26]
Geographical distribution varied, with most of the included studies stemming from Sierra Leone (n=23). Five were conducted in Guinea and seven in Liberia. Evidently, one key finding of this review is that the majority of qualitative literature originates from Western Urban Area, Sierra Leone. Table 3 outlines the geographical nature of all included studies. Regarding research design, numerous approaches were adopted. Case studies and rapid qualitative evaluations were frequently used, especially in terms of examining the association between health seeking behaviour and disease control [21, 22]. Cross-sectional approaches which focused on providing a snapshot within a specific geographical locale were also common [23]. Although not as prevalent, some ethnographic studies were also identified [24]. Likewise, in some instances, reference was made to a specific theoretical approach underpinning design [25].
Table 3
List of districts and countries covered by included studies
| Country | Regional districts researched: | No. of studies conducted in region: | Researched in: |
| Sierra Leone | Western Urban | 10 | [25], [27], [28-31], [32], [33], [34], [35] |
| Kambia | 7 | [36], [37], [30], [38], [32], [33], [39] | |
| Bo | 7 | [22], [40], [41], [42], [34], [43], [44] | |
| Port Loko | 6 | [21], [27], [29], [30], [38], [32] | |
| Moyamba | 6 | [40], [45], [30], [32], [46], [42] | |
| Western Rural | 4 | [29], [30], [32], [33] | |
| Kono | 4 | [30], [38], [32], [33] | |
| Tonkolili | 4 | [28], [29], [38], [33] | |
| Kenema | 4 | [40], [41], [47], [35] | |
| Bombali | 3 | [29], [31], [33] | |
| Koinadugu | 2 | [27], [45] | |
| Kailahun | 1 | [48] | |
| Pujehun | 1 | [40] | |
| Guinea | Région de Nzérékoré | 3 | [24], [49], [50] |
| Région de Conakry | 2 | [50], [51] | |
| Région de Kindia | 3 | [23], [50], [51] | |
| Région de Labé | 1 | [50] | |
| Région de Faranah | 1 | [50] | |
| Liberia | Montserrado County | 7 | [43, 44, 52-56] |
| Lofa | 1 | [55] | |
| Margibi | 1 | [55] | |
| Grand Cape Mount | 1 | [56] |
Every included study utilised at least one type of qualitative method (Table 4), with interviews (n=30), focus groups (n=23) and observational techniques (n=8) being the most popular. Some also opted for a mixed-method approach, utilising both qualitative and quantitative methods (n=4). Moreover, most studies triangulated between different data sources, gathering perspectives from different social groups like volunteers and community members. Only one opted for a more homogeneous approach, drawing from only one specific social group characteristic (i.e., community leaders) (n=1).
Table 4
Types of qualitative methods used in all studies
| Method | Used in: |
| Interviews (n = 30) | [21, 23-25, 27-31, 33-37, 39, 40, 42-52, 54-56] |
| Focus groups (n = 23) | [21, 22, 24, 25, 27, 29, 31-33, 36, 38, 39, 41, 42, 45, 47, 49, 51-56] |
| Observations (participatory research) (n = 8) | [21, 23, 37, 39, 40, 49, 51, 53] |
| Informal discussions (n = 4) | [33, 40, 46, 54] |
| Field notes (n = 2) | [28, 53] |
| Secondary/desk based (n = 3)[i] | [23, 50, 54] |
| Questionnaire (n = 1) | [21] |
| Mixed method (n = 4) | [30, 33, 45, 48] |
Quality of included studies was generally good, with the main issue being a lack of reflexivity. This is a key aspect to increasing the credibility of qualitative work, in which the researcher critically reflects upon their role in shaping the research project [57]; thus, this finding was problematic. Further, in some instances the process of data analysis clearly lacked detail, making it difficult to discern how rigorous the process was. Most concerningly, ethical approval for certain projects was not sought because primary data collection was considered to be part of a ‘broader disease response’ [49]. Taking these issues into consideration, it must be noted that this research was conducted in an unprecedented emergency with the main focus being on acute disease response where it may not have been possible to gain timely academic research ethics approval. Yet, future researchers must ensure rigorous analysis, quality and ethical protocols are still followed whenever conducting fieldwork in similar circumstances, in ensuring the best possible evidence informs practice.
Overall, six main- and five sub-themes relating to beliefs and/or practices that either hindered or promoted disease control were generated (Table 5). The reviewed evidence suggests that beliefs and/or practices relating to distrust, denial, fear and socio-cultural considerations hindered engagement with disease control. By contrast, experiencing the virus first-hand and seeing survivors leave treatment centres alive likely promoted the uptake of such measures. It should be noted that analytical theme titles were constructed and named relating to the inferred meaning prescribed to the reviewed data [20]. For instance, fear of healthcare referred to the perceived danger of specific healthcare associated objects (i.e., ambulances).
Table 5
Summary of themes generated via thematic synthesis
| Main Themes | Sub-Themes | Thematic/definitive example | |
| Beliefs/practices that hindered disease control | 1. Distrust of healthcare | a. Pre-existing climate of distrust | "A lot do not trust the medical people" [31] |
| 2. Denial and disbelief | / | "At first I did not believe in Ebola. Yes. Never. I didn't like talking about Ebola at first. When me and my friends gathered talking of Ebola, I just walked off saying, I'm not party to this, because Ebola is not real" [28] | |
| 3. Fear of healthcare | a. Never to return | "So, people decided 'well, let me die in my room.'' Because most people when they go [to the hospital], they will never come again" [25] | |
| b. Body and blood takers | "[They] are telling lies that [the vaccine] is Ebola, [it is here] to capture people, draw their blood, put it into a container and take it out. You see? They said they saw a lot of containers full of blood at the Airport, so that caused more fear" [39] | ||
| 4. Socio-cultural considerations | a. Burial practices: tensions with responders | "They were disrespecting the dead who were not buried properly, and I hated them for that reason" [47] | |
| b. Duty of care | "It will be impossible that my child or husband is sick, and I refuse to touch them. I do not have the courage or heart to do that" [53] | ||
| Beliefs/practices that promoted disease control | 1. Seeing is believing | / | "They only got it correct that there is Ebola when they started seeing...when the man died...when they saw it" [43] |
| 2. Survivors: beacons of hope | / | "At first, they were calling it 'death centre' because all those who were taken there died. But now we are seeing them going there and coming out alive" [32] |
‘Distrust of healthcare’ was one of the most prominent themes that arose from the examined literature. Regarding healthcare and disease control, distrust was associated with contact tracers [48], vaccine trials [37, 54], hospital services [31], community liaison personnel [47], Ebola Treatment Units (ETUs) [43], health messages [23] and chlorine/disinfection use [23, 35, 43]. Interestingly, in justifying their distrust, some participants cited anecdotal stories of maltreatment in healthcare settings, in which staff mistreated patients suffering from EVD [28, 44]. One narrated of a patient who:
“was not attended to. He was not given food, people used to put food in plastic and kicked towards him. Finally, he died. From that time, they lost trust” [44].
As such, a key theme that ran throughout all the aforementioned papers was a distinctive distrust of healthcare services. As one community liaison volunteer put it:
“they thought we were betraying them. They saw us as spies” [47].
From their secondary perspective, authors argued that such distrust stemmed not only from a dysfunctional healthcare system [28, 31, 42, 47] and poor government policy/control [22, 23, 28, 42, 47, 55, 56], but also from what was commonly termed a ‘pre-existing climate of distrust’ [23, 34, 37, 39, 43, 47, 52, 54-56]. Such a climate was moulded by years of colonial violence, corruption and war which fundamentally shaped how members of the general public throughout West Africa perceived healthcare. Some even suggested that such a climate played a role in facilitating denial of the virus [43], highlighting how it left:
“communities somewhat mistrusting, whereby survivors recalled a time early in the outbreak timeline when they and other community members suspected that Ebola was not real” [43].
This narrative surrounding a ‘pre-existing climate of distrust’ was mostly held for research conducted in Liberia [43, 52, 54-56] and Sierra Leone [34, 37, 39, 47], although similar comments were made regarding the Guinean context [23].
Although still a prevalent theme, ‘denial and disbelief’ was less common when compared to themes like ‘Distrust of healthcare’. Yet, it often interconnected with the latter themes and was mentioned by research conducted within Sierra Leone [25, 28, 30-32, 34, 39, 41, 43, 47, 48] and Liberia [52-56]. Often, beliefs surrounding denial centred around conspiracy theories. Within the Liberian context, some believed EVD was a biological weapon being used by “white people” to reduce Liberia’s population [54, 55]. Similar beliefs were identified in Sierra Leone, in which denial of the virus was often associated with political conspiracies [25, 47]. Ultimately, participants’ constructs revealed that such conspiracy narratives seemed to perpetuate denial until the disease was experienced first-hand, which is further discussed below.
Fear of healthcare played a multi-factorial role in hindering disease responses. This theme was most prevalent in Sierra Leone [21, 25, 27, 28, 30-35, 37, 39, 41-43, 45-48] although it was also mentioned by research conducted in Liberia [44, 52-55] and Guinea [23, 24, 49-51]. Primary constructs make it clear that healthcare services were typically associated with death and disappearance. Namely, ambulances were symbolically seen as objects of death [21, 25, 27, 30, 32, 35], as one participant explained:
“The sound, [makes siren sound], it’s like the siren is calling ‘I’m coming to kill you, kill you” [27].
Yet, it was not just ambulances that inspired fear, as chlorine use [32, 34, 35, 43, 47, 55], protective personal equipment (PPE) [21, 44, 48], and even hospitals [33, 41, 42, 45, 47], evoked feelings of fear.
Here, it is also important to touch on the sub-themes ‘never to return’ and ‘body and blood takers’. ‘Never to return’ was often associated with specific aspects of healthcare, like ambulances or ETUs. The examined literature narrated of people describing how loved ones were taken away by healthcare professionals and never seen again [21, 25, 27, 31, 34, 46]. Likewise, beliefs relating to blood and body part mining were prevalent, in which it was suspected that blood was being taken from suspected EVD patients and sold to Western elites [28, 39, 43, 48, 54]. In some extreme cases, participants knew of people who opted to die at home rather than be “drained of blood” at the hospital [28]. Secondary interpretations provided by study authors further reinforced these sub-themes, suggesting that such beliefs hindered control efforts [21, 24, 25, 28, 34, 42, 46, 49, 53, 54].
Socio-cultural considerations
Like distrust, denial and fear, the overstepping of socio-cultural considerations proved to be problematic. Our analysis generated two sub-themes related to this overarching theme, namely ‘burial practices: tensions with responders’ and ‘duty of care’. The sub-theme ‘burial practices: tensions with responders’, contains participant quotes which make it clear that during the outbreak the overstepping of traditional/cultural practices on the part of burial teams caused distress, especially during body transportation and burial [21, 22, 25, 27, 31, 35, 38, 41, 47, 48, 56]. Seeing the deceased being handled “like any animal” [22] was a distressing experience. Some highlighted that conflicts occurred on more than one occasion [25, 41]. Examples of such violations include the clash of gender funeral roles (i.e., males burying females) [21, 48], issues surrounding the use of body bags [21, 31, 41, 48] and the distinctive lack of praying during burial [21, 48]. In some instances, sick relatives were even hidden in order to avoid burial teams [27, 56].
Like with traditional burials, many participants saw caring for sick relatives as one’s duty [33, 38, 44, 47, 48, 53]. However, this ‘duty of care’ sometimes placed carers in danger and complicated health seeking behaviours. One study reports a participant from Kailahun District, Sierra Leone saying:
“It is our culture to touch people when they are sick, so if you don’t take people out of the village, people will touch them” [48].
Study authors further built on this point, arguing that West African culture emphasises compassionate care for the sick [44]. Such commitment to traditional care-giving roles likely hindered ETU use, due to bio-safety protocols which restricted physical contact with the infected [38, 49]. However, when disease responders took this duty of care into consideration when structuring treatment facilities, perceptions surrounding treatment centres became more positive [27, 38].
In contrast to the themes ‘denial’ and ‘distrust’, when EVD was encountered, its reality was no longer questioned. In one of the studies, this phenomenon was exemplified by the following quote from Sierra Leone:
“There is a saying, kill a dog before a dog, so that a dog will know that there is death. And some people began to see, and then they realise that Ebola is real” [28].
Such a portrayal of the transition from denial to acceptance was echoed throughout many primary accounts [21, 28, 34, 43, 47, 48]. Secondary interpretations from multiple authors further emphasised this vital role of ‘seeing is believing’ in challenging certain beliefs around EVD [28, 31, 34, 43, 48, 52, 55].
Experiencing the virus first hand was not the only means of promoting belief and behaviour change, as survivors also played a fundamental role in promoting disease control. This theme, entitled ‘survivors: beacons of hope’, captures how although some cases of stigma did exist [23, 24, 30-32, 44, 47, 54], overall survivors were critical in shifting perceptions away from beliefs centred on fear and denial. This theme ran throughout literature from Sierra Leone [21, 28, 30-32, 47, 48], Liberia [53, 55], and Guinea [49, 51]. According to participants, just seeing someone leave an ETU alive inspired hope, changing perceptions surrounding disease responders [21, 32, 47, 48, 55]. Some survivors even acknowledged that after seeking out treatment and surviving EVD, they became ‘role models’ for the fight against the virus [28, 30]. Thus, survivors were often involved in health messaging campaigns [28, 30-32, 47, 49, 53], and delegating infected people to treatment centres [48].
In order to gain a deeper appreciation of why certain beliefs and/or practices around EVD arose and how they shaped engagement with control measures, Hewlett’s ECA model is of importance. As previously highlighted, adopting such an ecological model in interpreting our findings connects our work to broader developments in the field of global health – which stress the vital role anthropological theory has in understanding health emergencies [10, 11].
Regarding our findings, take the aforementioned issues surrounding burial teams and the way in which traditional cultural practices and norms were overstepped. This finding, ‘burial practices: tensions with responders’, reflects the cultural component of the ECA model. Moreover, other themes, such as ‘fear of healthcare’ and ‘the duty of care’, highlight how Hewlett’s notion of culturally constructed niches, both in an external and internal sense, also hindered engagement with control measures [10]. Externally, the very structure and ‘mystery’ of healthcare services (i.e., ambulances or chlorine use) hindered treatment seeking behaviours due to fears surrounding death and disappearance. Further, internal culturally constructed niches, such as gender roles and one’s ‘duty to care’, on some occasions led to the avoidance of ETUs.
In terms of the evolutionary roots of certain beliefs, our findings seem to reinforce Hewlett’s framing of fear, which within the ECA framework is linked with human nature and biology [10]. Being afraid of entering an ambulance and never returning was a positive adaptive response to what many people felt was a death sentence. Likewise, the fear of being admitted to hospital also makes sense from a survival standpoint, given that nosocomial infection was common during the outbreak [58]. Yet, in thinking about the variety of ways fear was made manifest, it is also important to consider that such emotions are not restricted to one single domain, but interconnect with other parts of the framework. For instance, the fear of never returning was not only rooted in evolutionary instincts but was also mediated by cultural and ecological factors. In terms of cultural mediation, never returning home has implications for receiving a culturally appropriate burial [59]. Moreover, ecological factors relating to one’s proximity to a treatment centre, and the structure of the treatment centre itself, can also mediate fear [10].
It is important to acknowledge that, although Hewlett’s ECA approach provides a useful lens for interpreting our findings, one key limitation was identified. Given that emotions like fear and distrust are directly mediated by ecological factors, one would expect that the importance of social, political and historical forces would be highlighted as influencing such a component. After all, one’s proximity to a treatment centre and even the quality of care delivered within such a setting is directly related to resources a specific locality has, resources which are shaped by years of socio-political tensions. Yet, within his framework no attention is given to these determinants. Indeed, this critique connects to the caution raised at the start of this review, that placing too much focus on cultural or psychological manifestations of causality runs the risk of omitting the role social, political and historical factors had in exacerbating the outbreak [8].
Building from our synthesis, this limitation became even more apparent when considering a key sub-theme we generated, ‘pre-existing climate of distrust’. This finding further reiterates the argumentation developed in the latter paragraph, as author narratives stressed that years of colonial violence, corruption and war created fertile ground for distrust, denial and fear to surface across West Africa during the outbreak. Consequently, we present here an adapted model of Hewlett’s ECA approach, more suited to interpreting the findings of this review (Figure 2). Note the added component ‘historical, social and political forces’, which is contained within dashed boxes, outlining our suggested theoretical amendment. This illustrates how such factors shape the ecological context people inhabit, which includes healthcare facilities and disease response in general. Consequently, in such an ecology where public hospitals lack the most basic equipment yet nearby mining companies have access to appropriate medical care [8], it is no surprise that distrust was rampart during the outbreak. It should be noted other themes identified within this review are also outlined within the figure in bolded text.
ECA framework to human responses during EVD outbreaks, modified from Hewlett 2016 [10]
Although caution must be applied in drawing generalisations between our findings and other outbreaks (like the Severe Acute Respiratory Syndrome (SARS) coronavirus 2 pandemic), one key recommendation can still be made. Whatever the pathogen, policymakers and practitioners must focus on the wider social significance of clinical and behavioural interventions used during health emergencies. For instance, such reflective practice could take the form of opting for more ‘bottom up’ communication campaigns rather than adopting a top down ‘one size fits all’ approach [60]. Social scientists could also collaborate with clinicians, in ensuring that relevant interventions do not overstep deeply embedded social practices [60]. As learned from the West African EVD outbreak, understanding the different meanings surrounding disease control is difficult, but has shown to be worthwhile if any serious community engagement is to be developed.
Regarding review methodology, there are some limitations which should be considered. First, issues surrounding generalisability are evident. This review adopted a broad approach in taking literature from across West Africa; therefore, findings and theoretical conclusions must be cautiously applied to other contexts. Further, the inter-transferability of the findings drawn within and between the latter countries raises the same issue, as a broad conceptual framing of disease control was used in drawing comparisons. However, given the geographical heterogeneity of the outbreak, it would have been ill-judged to simply focus on one intervention, community or country, as doing so would have restricted our ability to conduct any form of cross-cultural analysis. The point was to move away from micro level programme evaluation, in taking a holistic (and therefore theoretical) approach in understanding why similar strands of resistance arose throughout different parts of West Africa. This was achieved when we moved away from findings from individual studies and into the realm of synthesis [20].
Second, among and within Sierra Leone, Guinea and Liberia, there appears to be some research disparity. Future researchers must narrow this gap between and within these three countries in strengthening the qualitative evidence base prior to future outbreaks. This could include utilising different data visualisation techniques in geographically mapping the literature, showing which areas require further research. Lastly, grey literature, such as reports produced by the WHO were not included. Future researchers can also build on this limitation by incorporating multiple types of literature in their reviews of the qualitative EVD evidence base.
This review aimed to understand what role certain beliefs and/or practices – held by the general public in Sierra Leone, Liberia, and Guinea – played in either hindering or promoting disease control during the West African EVD outbreak. Building on these findings, we also aimed to make a novel theoretical contribution to an existing framework (Hewlett’s ECA approach) in order to advance insights into why resistance to disease control arises. Regarding the former, it was identified that beliefs and/or practices relating to distrust, fear of healthcare, certain socio-cultural considerations and denial, hindered the uptake of control measures, whereas experiencing the virus first-hand and interacting with survivors increased engagement. Additionally, in terms of theoretical considerations, we amended Hewlett’s ECA framework augmenting it with insights into how wider historic, social and political factors shape behaviour during outbreaks.
Overall, this review provides contextual insights for policy and practice in relation to good practices when dealing with EVD outbreaks, both in a specific contextual (West Africa) and more mechanistic (practical transferability) sense. Policymakers and practitioners need to reflect upon how outbreaks exacerbate complex social dynamics which, in turn, determines whether or not control efforts are successful. Even something as simple as chlorine use can potentially have serious ramifications for health seeking behaviour if not understood and implemented in a context-sensitive manner. Therefore, our revised model of Hewlett’s ECA approach could serve as a guiding framework in helping policymakers and practitioners (both throughout West Africa and beyond) devise interventions which do not overstep such boundaries.
Finally, the findings of this review have also highlighted the need for more qualitative research to be undertaken throughout Liberia and Guinea. Such research, even when conducted during health emergencies, must be as transparent as possible. This means reflexivity must be practiced whilst ensuring that appropriate ethical and research procedures are followed. This, alongside further evidence reviews that synthesise both more practical and academic literature, will ensure a more solid evidence base exists which would help guide response efforts prior or during future EVD outbreaks.
All authors would like to thank Sonny Maley from the University of Glasgow library in helping formulate the search strategy for this review.
Author TB is the primary author of this manuscript, because of his critical role during every stage of the research project (i.e., from research question formulation to theoretical development and argumentation). Secondary author TVB played a crucial role in revising the manuscript prior to publication by re-editing and proof-reading it multiple times. Author NRC played a role in review design, screening, theoretical development, and proof-reading. Lastly, Author VW conducted further handsearching and was involved throughout the screening process.
The authors have no competing interests to declare.
Supplement 1. Prisma Checklist
Supplement 3. Search strategies used
Supplement 4. Modified Critical Appraisal Skills Programme (CASP) checklist
Supplement 5. Data extraction sheets
Supplement 6. Phase 2 Exclusions
1. Frontières MS. Pushed to the limit and beyond: a year into the largest ever Ebola outbreak 2015.
2. Pourrut X, Kumulungui B, Wittmann T, Moussavou G, Délicat A, Yaba P, et al. The natural history of Ebola virus in Africa. Microbes and infection. 2005;7(7-8):1005-14.
3. Baize S, Pannetier D, Oestereich L, Rieger T, Koivogui L, Magassouba NF, et al. Emergence of Zaire Ebola virus disease in Guinea. New England Journal of Medicine. 2014;371(15):1418-25.
4. Control CfD. 2014-2016 Ebola outbreak in West Africa 2019 [updated 2019. Available from: https://www.cdc.gov/vhf/ebola/history/2014-2016-outbreak/index.html.
5. Team WER. Ebola virus disease in West Africa—the first 9 months of the epidemic and forward projections. New England Journal of Medicine. 2014;371(16):1481-95.
6. Buseh AG, Stevens PE, Bromberg M, Kelber ST. The Ebola epidemic in West Africa: Challenges, opportunities, and policy priority areas. Nursing Outlook. 2015;63(1):30-40.
7. Frankfurter R, Kardas-Nelson M, Benton A, Barrie MB, Dibba Y, Farmer P, et al. Indirect rule redux: the political economy of diamond mining and its relation to the Ebola outbreak in Kono district, Sierra Leone. Review of African Political Economy. 2018;45(158):522-40.
8. Richardson ET, Barrie MB, Kelly JD, Dibba Y, Koedoyoma S, Farmer PE. Biosocial approaches to the 2013-2016 Ebola pandemic. Health and human rights. 2016;18(1):115.
9. Control CfD. The Social-Ecological Model: A Framework for Prevention 2022 [updated 18/01/2022. Available from: https://www.cdc.gov/violenceprevention/about/social-ecologicalmodel.html.
10. Hewlett BS. Evolutionary cultural anthropology: containing Ebola outbreaks and explaining hunter-gatherer childhoods. Current Anthropology. 2016;57(S13):S27-S37.
11. Stellmach D, Beshar I, Bedford J, Du Cros P, Stringer B. Anthropology in public health emergencies: what is anthropology good for? BMJ global health. 2018;3(2):e000534.
12. Hewlett BS, Amola RP. Cultural contexts of Ebola in northern Uganda. Emerging infectious diseases. 2003;9(10):1242.
13. Abramowitz SA, Hipgrave DB, Witchard A, Heymann DL. Lessons from the West Africa Ebola epidemic: A systematic review of epidemiological and social and behavioral science research priorities. The Journal of infectious diseases. 2018;218(11):1730-8.
14. Johnson GA, Vindrola-Padros C. Rapid qualitative research methods during complex health emergencies: a systematic review of the literature. Social Science & Medicine. 2017;189:63-75.
15. Muzembo BA, Ntontolo NP, Ngatu NR, Khatiwada J, Suzuki T, Wada K, et al. Misconceptions and Rumors about Ebola Virus Disease in Sub-Saharan Africa: A Systematic Review. International journal of environmental research and public health. 2022;19(8):4714.
16. PRISMA. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2021 [Available from: https://prisma-statement.org/.
17. Butler A, Hall H, Copnell B. A guide to writing a qualitative systematic review protocol to enhance evidence‐based practice in nursing and health care. Worldviews on Evidence‐Based Nursing. 2016;13(3):241-9.
18. Stern C, Jordan Z, McArthur A. Developing the review question and inclusion criteria. AJN The American Journal of Nursing. 2014;114(4):53-6.
19. Saini M, Shlonsky A. Systematic synthesis of qualitative research: OUP USA; 2012.
20. Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC medical research methodology. 2008;8(1):1-10.
21. Carter SE, O'Reilly M, Walden V, Frith-Powell J, Umar Kargbo A, Niederberger E. Barriers and Enablers to Treatment-Seeking Behavior and Causes of High-Risk Practices in Ebola: A Case Study From Sierra Leone. Journal of Health Communication. 2017;22(sup1):31-8.
22. Lee-Kwan SH, DeLuca N, Bunnell R, Clayton HB, Turay AS, Mansaray Y. Facilitators and Barriers to Community Acceptance of Safe, Dignified Medical Burials in the Context of an Ebola Epidemic, Sierra Leone, 2014. Journal of Health Communication. 2017;22(sup1):24-30.
23. Thiam S, Delamou A, Camara S, Carter J, Lama EK, Ndiaye B, et al. Challenges in controlling the Ebola outbreak in two prefectures in Guinea: why did communities continue to resist? The Pan African medical journal. 2015;22 Suppl 1:22.
24. Manca MC. ‘Yassaba’ or the Fear of Being Abandoned: Health promotion messages and local meanings in Guinea. 2017.
25. Murray RT, Drew LB, Memmott C, Bangura Y-M, Maring EF. A community’s experience during and after the Ebola epidemic of 2014—2016 in Sierra Leone: A qualitative study. PLOS Neglected tropical diseases. 2021;15(2):e0009203.
26. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Systematic reviews. 2021;10(1):1-11.
27. Carter SE, O'Reilly M, Frith-Powell J, Umar Kargbo A, Byrne D, Niederberger E. Treatment Seeking and Ebola Community Care Centers in Sierra Leone: A Qualitative Study. Journal of Health Communication. 2017;22(sup1):66-71.
28. Gray N, Stringer B, Bark G, Heller Perache A, Jephcott F, Broeder R, et al. 'When Ebola enters a home, a family, a community': A qualitative study of population perspectives on Ebola control measures in rural and urban areas of Sierra Leone. PLoS Neglected Tropical Diseases [electronic resource]. 2018;12(6):e0006461.
29. Jalloh MF, Jalloh MB, Albert A, Wolff B, Callis A, Ramakrishnan A, et al. Perceptions and acceptability of an experimental Ebola vaccine among health care workers, frontline staff, and the general public during the 2014-2015 Ebola outbreak in Sierra Leone. Vaccine. 2019;37(11):1495-502.
30. Karafillakis E, Jalloh MF, Nuriddin A, Larson HJ, Whitworth J, Lees S, et al. ‘Once there is life, there is hope’Ebola survivors' experiences, behaviours and attitudes in Sierra Leone, 2015. BMJ global health. 2016;1(3):e000108.
31. Kinsman J, de Bruijne K, Jalloh AM, Harris M, Abdullah H, Boye-Thompson T, et al. Development of a set of community-informed Ebola messages for Sierra Leone. PLoS Neglected Tropical Diseases [electronic resource]. 2017;11(8):e0005742.
32. Nuriddin A, Jalloh MF, Meyer E, Bunnell R, Bio FA, Jalloh MB, et al. Trust, fear, stigma and disruptions: community perceptions and experiences during periods of low but ongoing transmission of Ebola virus disease in Sierra Leone, 2015. BMJ Glob Health. 2018;3(2):e000410.
33. Pronyk P, Rogers B, Lee S, Bhatnagar A, Wolman Y, Monasch R, et al. The Effect of Community-Based Prevention and Care on Ebola Transmission in Sierra Leone. American journal of public health. 2016;106(4):727-32.
34. Yamanis T, Nolan E, Shepler S. Fears and misperceptions of the Ebola response system during the 2014-2015 outbreak in Sierra Leone. PLoS neglected tropical diseases. 2016;10(10):e0005077.
35. Jalloh MF, Kinsman J, Conteh J, Kaiser R, Jambai A, Ekström AM, et al. Barriers and facilitators to reporting deaths following Ebola surveillance in Sierra Leone: implications for sustainable mortality surveillance based on an exploratory qualitative assessment. BMJ open. 2021;11(5):e042976.
36. Dada S, McKay G, Mateus A, Lees S. Lessons learned from engaging communities for Ebola vaccine trials in Sierra Leone: reciprocity, relatability, relationships and respect (the four R's). BMC Public Health. 2019;19(1):1665.
37. Enria L, Lees S, Smout E, Mooney T, Tengbeh AF, Leigh B, et al. Power, fairness and trust: understanding and engaging with vaccine trial participants and communities in the setting up the EBOVAC-Salone vaccine trial in Sierra Leone. BMC Public Health. 2016;16(1):1140.
38. Mokuwa EY, Maat H. Rural populations exposed to Ebola Virus Disease respond positively to localised case handling: Evidence from Sierra Leone. PLoS neglected tropical diseases. 2020;14(1):e0007666.
39. Tengbeh AF, Enria L, Smout E, Mooney T, Callaghan M, Ishola D, et al. "We are the heroes because we are ready to die for this country": Participants' decision-making and grounded ethics in an Ebola vaccine clinical trial. Social Science & Medicine. 2018;203:35-42.
40. Bonwitt J, Dawson M, Kandeh M, Ansumana R, Sahr F, Brown H, et al. Unintended consequences of the ‘bushmeat ban’in West Africa during the 2013–2016 Ebola virus disease epidemic. Social Science & Medicine. 2018;200:166-73.
41. McMahon SA, Ho LS, Scott K, Brown H, Miller L, Ratnayake R, et al. "We and the nurses are now working with one voice": How community leaders and health committee members describe their role in Sierra Leone's Ebola response. BMC Health Services Research. 2017;17(1):495.
42. Richards P, Mokuwa GA, Vandi A, Mayhew SH. Re-analysing Ebola spread in Sierra Leone: The importance of local social dynamics. PLoS ONE. 2020;15(11).
43. Schwerdtle P, De Clerck V, Plummer V. Survivors' perceptions of public health messages during an Ebola crisis in Liberia and Sierra Leone: An exploratory study. Nursing & Health Sciences. 2017;19(4):492-7.
44. Schwerdtle PM, De Clerck V, Plummer V. Experiences of Ebola Survivors: Causes of Distress and Sources of Resilience. Prehospital & Disaster Medicine. 2017;32(3):234-9.
45. Elston J, Moosa A, Moses F, Walker G, Dotta N, Waldman RJ, et al. Impact of the Ebola outbreak on health systems and population health in Sierra Leone. Journal of Public Health. 2016;38(4):673-8.
46. Parker M, Hanson TM, Vandi A, Babawo LS, Allen T. Ebola and public authority: saving loved ones in Sierra Leone. Medical Anthropology. 2019;38(5):440-54.
47. Richards P, Mokuwa E, Welmers P, Maat H, Beisel U. Trust, and distrust, of Ebola Treatment Centers: A case-study from Sierra Leone. PLoS One. 2019;14(12):e0224511.
48. Caleo G, Duncombe J, Jephcott F, Lokuge K, Mills C, Looijen E, et al. The factors affecting household transmission dynamics and community compliance with Ebola control measures: a mixed-methods study in a rural village in Sierra Leone. BMC Public Health. 2018;18(1):248.
49. Carrion Martin AI, Derrough T, Honomou P, Kolie N, Diallo B, Kone M, et al. Social and cultural factors behind community resistance during an Ebola outbreak in a village of the Guinean Forest region, February 2015: a field experience. International Health. 2016;8(3):227-9.
50. Kodish SR, Rohner F, Beauliere J-M, Daffe M, Ag Ayoya M, Wirth JP, et al. Implications of the Ebola virus disease outbreak in Guinea: Qualitative findings to inform future health and nutrition-related responses. PloS one. 2018;13(8):e0202468.
51. Ronse M, Mari Saez A, Gryseels C, Bannister-Tyrrell M, Delamou A, Guillard A, et al. What motivates Ebola survivors to donate plasma during an emergency clinical trial? The case of Ebola-Tx in Guinea. PLoS Neglected Tropical Diseases [electronic resource]. 2018;12(10):e0006885.
52. Abramowitz S, McKune SL, Fallah M, Monger J, Tehoungue K, Omidian PA. The Opposite of Denial: Social Learning at the Onset of the Ebola Emergency in Liberia. Journal of Health Communication. 2017;22(sup1):59-65.
53. Abramowitz SA, McLean KE, McKune SL, Bardosh KL, Fallah M, Monger J, et al. Community-centered responses to Ebola in urban Liberia: the view from below. PLoS Neglected Tropical Diseases [electronic resource]. 2015;9(4):e0003706.
54. Alenichev A. ‘We will soon be dead’: stigma and cascades of looping effects in a collaborative Ebola vaccine trial. Critical public health. 2021;31(1):55-65.
55. Ali SH, Wells K, Rose JR. Contextualizing Risk Perception and Trust in the Community-Based Response to Ebola Virus Disease in Liberia. Int J Environ Res Public Health. 2021;18(6).
56. Pellecchia U, Crestani R, Decroo T, Van den Bergh R, Al-Kourdi Y. Social Consequences of Ebola Containment Measures in Liberia. PLoS ONE [Electronic Resource]. 2015;10(12):e0143036.
57. Patnaik E. Reflexivity: Situating the researcher in qualitative research. Humanities and Social Science Studies. 2013;2(2):98-106.
58. Dunn AC, Walker TA, Redd J, Sugerman D, McFadden J, Singh T, et al. Nosocomial transmission of Ebola virus disease on pediatric and maternity wards: Bombali and Tonkolili, Sierra Leone, 2014. American Journal of Infection Control. 2016;44(3):269-72.
59. Hewlett BS, Hewlett BL. Ebola, culture and politics: the anthropology of an emerging disease: Cengage Learning; 2007.
60. Anoko JN, Barry BR, Boiro H, Diallo B, Diallo AB, Belizaire MR, et al. Community engagement for successful COVID-19 pandemic response: 10 lessons from Ebola outbreak responses in Africa. BMJ Global Health. 2020;4(Suppl 7):e003121.
1 Secondary/desk based refers to research which utilises pre-existing data, and doesn’t involve the creation of new ‘primary’ data (i.e., policy analysis or systematic reviews)