Watching Brief
Japanese Encephalitis Outbreak in South-Eastern Australia, 2022
| Date of first report of the outbreak | Animal cases (Pigs): |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Disease or outbreak | Japanese encephalitis virus (JEV) is a single-strand, positive-sense RNA virus of the genus Flavivirus, family Flaviviridae 8). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Origin (country, city, region) | JEV is prevalent in tropical and subtropical parts of Asia and parts of the Pacific rim (8). It was first reported in Japan in 1859, and remains one of the most important causes of viral encephalitis in Asia, with approximately 68,000 clinical cases each year (9). |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Suspected Source (specify food source, zoonotic or human origin or other) | JEV is a mosquito-borne disease. People and animals become infected by the bite of infected mosquitoes. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Date of outbreak beginning | Animal case (pig): 19/1/22 (1) |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Date outbreak declared over | Outbreak is ongoing |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Affected countries & regions | States of south-eastern Australia |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Number of cases (specify at what date if ongoing) | 24 confirmed cases, 11 probable cases and 3 deaths, as of 4 April 2022 (table 1) (11).
Table 1 Number of cases by state
Laboratory diagnosis is confirmed through testing for:
Probable cases are defined as cases that have been linked epidemiologically and/or have symptoms of the disease and have laboratory evidence which is indicative of JEV, but cannot entirely rule out other related flaviviruses like Murray Valley Encephalitis (MVE) (11). |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Clinical features | In most cases, infection with JEV is asymptomatic, however in rare cases (less than 1%) it can cause severe illness with encephalitis and neurological complications (15). Incubation period: Severe illness can occur 5-15 days after infection, and presents with sudden onset of fever, headache, vomiting and convulsions (16). Elderly people and children under 5 are most at risk of severe illness, with children most likely to develop seizures (17). Natural infection confers lifelong immunity (18). |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Mode of transmission (dominant mode and other documented modes) | JEV is transmitted to humans through the bite of infected Culex species mosquitoes. The virus exists in a zoonotic cycle between waterbirds and mosquitoes, which commonly use the water for larval development (8). Other mammals can become infected, including horses and humans, however these are “dead-end” hosts, as they do not replicate enough of the virus in the blood stream to transmit to a feeding mosquito (16). Domestic pigs have very high (>90%) rates of infection with JEV, and are important amplifying hosts, with high levels of the virus sufficient to infect mosquitoes and continue transmission of the virus (8). Domestic pigs have a high annual turnover, therefore increasing susceptibility (8). The Culex tritaeniorhynchus is the predominant mosquito vector established in South-East Asia (19). This species was detected in Australia in the Darwin and Katherine regions of the Northern territory in February and May, 2020 and is likely established in northern Australia (20). The vector competence of Culex annulirostris has been identified as the primary vector in the transmission of JEV in the Torres Strait Islands, and in Papua New Guinea (21, 22). It is morphologically and ecologically similar to the C. tritaeniorynchus, and is widely established throughout Australia (21). C. annulirostris is reported to feed mainly on wallabies and other macropods, however, will feed on birds and pigs when greater numbers are available (8, 23) . In tropical areas the zoonotic cycle between mosquitos, birds and pigs will happen continuously (21). In more temperate areas, high levels of rainfall, such as has occurred along the east coast of Australia early in 2022, will increase mosquito populations and potentially allow infection to build up in waterbirds and then pigs, causing risk of JEV to humans exposed to infected mosquitos (21). |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Demographics of cases | Table 1 Demographic details of cases in Australia (current outbreak as of 7 April 2022)
*VIC - All cases have spent time around the Murray River area, and several had extensive mosquito exposure prior to illness onset
Figure 1
JEV in Australia as of 7 April 2022 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Case fatality rate | In current outbreak, there is 3 deaths resulting in a case fatality rate of 9% (3/35). It has been reported that 1 in 4 cases are fatal (16). |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Complications | Encephalitis (inflammation of the brain) develops in less than 1% of human cases. For these cases, between 20-30% are fatal, and up to 50% of those who survive experience ongoing neurological deficits and/or psychiatric illness (17) . |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Available prevention | Prevention includes mosquito surveillance and control measures and the roll out of vaccines to those identified as at direct risk (38). Avoiding mosquito bites is important for all in affected areas, including use of insect repellent, long clothing, and controlling mosquito populations indoors through use of screens on windows and doors (39). Vaccination In endemic countries such as those in South East Asia, vaccinations are prioritised for children under five years, as the majority of the population have been exposed to JEV previously (43). In Australia, the entire population is naïve to the virus, therefore priority must be given to those at risk of both exposure and severe disease (43). Demographics show that majority of cases are occurring around the affected piggeries where there is exposure to mosquitoes, and in the older age group (43). Therefore, the current vaccination roll out has been targeted to those groups (42, 43). |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Available treatment | There is no cure and supportive treatments are the only option - rest, fluids, and use of pain relievers and medication to reduce fever for symptom relief (17). |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
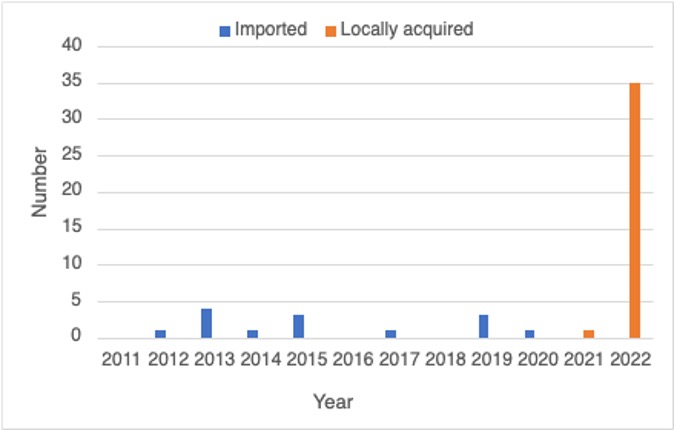
| Comparison with past outbreaks | Previous human cases in Australia In 1998, a further outbreak occurred on the Torres Strait Island, with two clinical human cases reported, including one in northern Queensland (23). There was further serological evidence of JEV in pigs in 2000 in the Torres Strait and Cape York. Mosquito-based surveillance in northern Australia since 2012 has not shown evidence of JEV (8). Japanese encephalitis is a notifiable disease in Australia (45). Since 2011 there have been sporadic imported cases reported in Australia (Table 1), with no evidence of ongoing transmission (46). In April 2021, there was one case reported on the Tiwi Islands, of JEV Genotype 4, likely carried over from Papua New Guinea, where genotype 4 is dominant (18). This was the first locally acquired case since 1998 (47).
Figure 2
Notified cases of Japanese Encephalitis in Australia |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Unusual features | 1. Geographic distribution: It has been the first JEV outbreak in mainland Australia. JEV has not been detected in mosquitos, animals or humans in south-eastern Australia previously (41). 2. Epidemic intensity: It is unusual to see the obviously higher number of human cases in 2022 in Australia, with only one case in northern mainland Australia and very few in the Torres Strait previously. Part of the government response is to undertake widespread testing of asymptomatic people in affected areas to determine the distribution of the disease in the human population (41). |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Critical analysis | Japanese Encephalitis is occasionally detected in northern Australia, in the Torres Strait region, but has not previously been detected below Cape York, with no established transmission recorded on mainland Australia (1). Due to this, it took several weeks for authorities to consider testing for JEV when investigating increased stillbirths in piggeries in QLD, NSW and VIC (48). When widespread testing took place, a large outbreak was discovered, with JEV now identified in at least 24 commercial pig farms across QLD, NSW, VIC and SA (49). Culex mosquitos are the main vectors of JEV. The main vector for JEV is Culex tritaeniorhynchus which had been absent from Australia until 2020, when it was detected in 19 female mosquito specimens in the Darwin and Katherine regions of the Northern Territory, Australia (20). It is possible Culex tritaeniorhynchus has become established in Australia and spread to the Southeast. Of the more common Culex species detected in Australia, there are five Culex species (Culex annulirostris, Culex australicus, Culex fergusoni, Culex globocoxitus, Culex quinquefasciatus) widespread in Southern Australia (50). The Culex annulirostris is documented as the dominant species from mid-spring to late-autumn in Southern Australia (51), particularly in Murray-Darling river drainage basin in QLD, NSW, VIC and SA (21, 52). The species of mosquito involved in transmission has not yet been identified, however, Culex annulirostris is considered to be the most likely vector in this outbreak (18, 22, 47). Culex annulirostris is associated with freshwater habitats including wetlands and flooded areas (22, 52-54). This species of mosquito is widespread across Australia, and is particularly abundant in late summer (52, 53). It lays eggs in standing water and can be dispersed up to 12km from larvae, although 5km is most common. It is an opportunistic feeder on a wide range of animals including birds and pigs (53). Culex annulirostris can transmit a wide range of arboviruses, including JEV, with an incubation period of seven to ten days post-infection web (53, 55). It has been previously reported that JEV isolates were identified in members of the Culex species while sampling mosquito populations in Badu Island in 1998 (55). Conditions leading to the emergence of JEV in southeastern Australia include above average rainfall and higher average temperatures which may have contributed to the spread of the disease through migration of water birds and increased mosquito populations (1). Climate change has been leading to hotter temperatures in temperate areas and extending the areas in which mosquitoes can thrive. The ‘La Nina’ event that emerged in the Pacific contributed to unusually high rainfall in Australia in 2021, which has also been shown to boost mosquito populations due to presence of large bodies of stagnant water which facilitates breeding. It has also been demonstrated that climate change has led to mosquito vectors invading higher elevations and latitudes (54). Water birds infected with the virus may have migrated into Northern Australia, and then been able to come south through waterways into South Eastern Australia, attracted by the availability of water (47, 54). These birds are likely reservoirs of JEV, with local mosquito populations feeding on infected waterbirds before spreading JEV to pigs and people (18, 47) and contributing to the emergence of this virus in South Eastern Australia. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Key questions | How did JEV become established on the mainland of Australia? What changes in vector distribution may account for this? Since it was first identified in Australia in 2021, is culex tritaeniorhynchus responsible for the epidemic? What preventive measures can be taken for prevention and control of human and non-human outbreaks? What will be the most effective vaccination strategy - at-risk population or targeted population and age groups etc? In the meantime, are there any increased reports of other mosquito-borne diseases in South-eastern Australia? |