The Coronavirus disease 2019 (COVID-19) is a communicable respiratory infection that continues to affect global health since its emergence in Wuhan City, China on 29 December, 2019 (1). As of 22nd May, 2022 an estimated 522 million cases and 6 million deaths have been reported in 255 countries (2). The African continent accounts for 3% of reported cases (5,911,505) and deaths (142, 417) of the global total. Since the onset, at least 54 (98%) of the Africa Union (AU) member States have experienced a second wave, 43 (78%) experienced a third wave and 7 (13%) have experienced fourth wave of COVID-19 cases (3). In Nigeria, the index case was reported on 27th February, 2020. Since then, a total of 203,991 confirmed cases and 2,672 deaths have been reported (4). Ondo State in southwest Nigeria is currently ranked the ninth state most affected by COVID-19, with a cumulative 3968 confirmed cases and 71 deaths reported from the 18 local government areas (LGAs) in the state as of 20th August, 32021 (5).
In response to the COVID-19 pandemic, the Nigeria Centre for Disease Control (NCDC), with significant collaborations from partners including the World Health Organization, have implemented a wide range of public health measures to prevent, contain and control SARS-COV-2 transmission. Measures implemented included complete or partial lockdowns, travel bans, restrictions on mass gatherings, home quarantines within communities, social distancing measures, personal protective actions, and use of other non-pharmaceutical measures (6). Based on the lessons learnt from the Ebola Virus Disease (EVD) outbreak, the NCDC and its partners have supported the 36 states of Nigeria, including the Federal Capital Territory, to implement the Incidence Management System through activation of the Public Health Emergency Operation Center (PHEOC) and trained rapid response teams (7). In addition, the agency provided relevant public health advice to Nigerians, built capacity for contact tracing and case management, and strengthened laboratory diagnostic capacity by establishing 84 molecular laboratories across the states (8).
However, COVID-19 testing has not been optimal or in keeping with most high-income countries. In Ondo State, only 22,263 were tested as of the end of March 2021. The number of COVID-19 tests conducted decreased from 1080 to 225 cases tested between 1st February to 21st March, 2021, with only two out of 21 sample collection sites active at the end of the period. Similarly, the case to contact ratio for January to March 2021 remained consistently low at 1:2 (3334 cases/1414 contacts) in Epi week 11, 2021. During the early period of the outbreak, the COVID-19 response was centralized, with response teams consisting of state-level officers. The testing, case management, and contact tracing were not integrated into the essential healthcare services at the health facility level, and there was no coordination of the response activities at the LGA level. Therefore, the World Health Organization State field office provided technical support to the state PHEOC to implement interventions aimed at integrating COVID-19 sample collection into the essential services in healthcare facilities and strengthening contact tracing and coordination meetings in three hotspot LGAs. This paper provides a description of the interventions, outcomes and lessons learnt to further guide outbreak response activities.
This is a health facility and community-based intervention implemented in Ondo State as part of outbreak response to COVID-19 pandemic from 24th May to 23rd August, 2021. Ondo State is located in the Southwest of Nigeria and has the capital at Akure. It lies between longitudes 4.0151°E and 6.0001°E of the Greenwich median and latitudes 5.0451°N and 7.0451° N, which are to the North of the equator in the Southwestern geopolitical zone of the country. It is bounded to the east by Edo and Delta State, to the North by Ekiti and Kogi States and Bight of Benin and the Atlantic Ocean to the South. The State has a surface area of approximately 15,317 square kilometers, with a projected population of 5,361, 295 in 2021 (annual growth rate of 3% based on the 2006 population census) (9).
Ondo State consists of 18 local government areas (LGAs) divided into 3 senatorial districts namely Ondo Central, North and South. On 3rd of April 2020, the index COVID-19 case in the state was reported in Akure South LGA. Since then, all 18 LGAs have reported a confirmed COVID-19 case, with three LGAs-Akure South, Akure North and Owo being hotspot LGAs. The LGAs were categorized as hot spot LGAs because they consistently had >15 active cases and > 5% test positivity criteria over several epidemiological weeks. The LGAs have a total of 34 wards: Akure South- 11, Akure North -12 and Owo -11 wards.
On 30th of March 2020, the Ondo State Ministry of Health received an alert from clinicians at a government-owned hospital in Akure Ondo State about a suspected COVID-19 case, who was a 34-year-old male with recent travel history to India. The index case arrived in Ondo State on 21st of March 2020 and presented with cough, sore throat and running nose at the hospital. Field investigations were conducted by the State Rapid Response Team (RRT) to investigate and implement public health response. Nasopharyngeal and oropharyngeal samples of the case were taken for laboratory confirmation and returned positive on 3rd April, 2020.
The State continued to use the existing Incident Management System (IMS) modeled after the Emergency Operations Center (EOC) for the control and management of Ebolavirus outbreak in Nigeria to respond to additional COVID-19 cases (10). Important EOC pillars or groups which included coordination, surveillance, risk communication or community mobilization, case management, infection prevention and control, and logistics were reactivated and functioned centrally at the state level, with minimal activity at the LGA or ward level. The state RRT members were the main actors involved in case investigation, contact tracing and follow-up, and samples collection and transportation across all 18 LGAs to designated state molecular laboratories for polymerase chain reaction (PCR) test. Despite the efforts of the state team, suboptimal testing was observed in the state, with a drastic reduction in the number tested from 7th March (285 cases) to 16th May (31 cases) 2021.
The World Health Organization field office provided technical support to Ondo State to strengthen decentralization of sample collection, contact tracing, home-based care monitoring of active cases and coordination at three hot spot LGAs between 24th May to 23rd August, 2021.
Initially, COVID-19 sample collection was done by trained laboratory staff in two collection sites at the accredited molecular laboratories in Ondo State. In affected communities, nasopharyngeal and oropharyngeal swabs of suspected cases and contacts were collected by the trained Diseases Surveillance and Notification Officers (DSNOs) at the state and LGA levels, and transported to functional public health laboratory at Federal Medical Center (FMC), Owo and the Infectious Disease Hospital (IDH), Akure for testing.
During case investigation, three categories of case definitions for COVID-19 were used to guide outbreak investigation according to the NCDC guidelines.
Suspected case: This category of case definition was further simplified into four forms, and they are; (1) patient with acute respiratory illness including fever and at least one sign/symptom of respiratory disease and a history of travel to or residence in a country/area or territory reporting local transmission of COVID-19 disease during the 14 days prior to symptom onset; or (2) a patient/health care worker with any acute respiratory illness and has been in contact with a confirmed COVID-19 case in the last 14 days prior to the onset of symptoms; or (3) a patient with a severe acute respiratory infection (fever and at least one sign/symptom of respiratory disease (e.g., cough, shortness of breath) and requiring hospitalization and with no other aetiology that fully explains the clinical presentation (11).
Confirmed case: A person with laboratory confirmation of COVID-19 infection, irrespective of clinical signs and symptoms.
Probable case: Any suspected case for whom testing for COVID-19 is indeterminate test result or for whom testing was positive on a pan-coronavirus assay.
Contact: A contact is defined as anyone who has face-to-face contact with a probable or confirmed case within 1 meter and for more than 15 minutes, direct physical contact with a probable or confirmed case, and/or direct care for a patient with probable or confirmed COVID-19 without the use of proper personal protective equipment 2 days before and within 14 days after the onset of symptoms of a probable or confirmed case.
Suspected cases were identified in the communities and health facilities through various channels such as self-reports, clinicians’ referrals, calls from communities to hotlines and follow-up investigation by the State RRT, or active surveillance, and contacts of confirmed cases under follow-up management.
To scale up sample collection in the state, the WHO supported the government to establish 103 COVID-19 sample collection sites in selected primary, secondary, tertiary and private health facilities across the 34 wards in 3 hotspot LGAs using the existing laboratory and surveillance structure. A total of 103 government-paid laboratory technicians (1 per health facility) and 18 LGA DSNOs were identified and trained on case investigation, sample collection, storage, transportation as well as the use of contact tracing forms, with key variables such as name, age, gender, exposure and quarantine details included in the form. Due to inadequate specimen carriers for storage and transportation of samples at the health facilities, provision was made for temporary storage containers and icepacks to store samples at the health facilities before transporting to the molecular laboratory for testing.
In addition, one sample collector/healthcare worker in a health facility within a ward in an LGA, had the responsibility of going to other designated health facilities within the ward to collect stored samples and to transport them to the office of the LGA DSNO daily. At the LGA Primary Health Care office, the DSNOs and assistants take these collated samples within the LGA to the State reference molecular laboratory daily for testing. Three LGA supervisors (1 per LGA) conducted supportive supervision to the sample collection sites, ensuring adherence to the recommended NCDC guidelines for sample collection and transportation. The KoboCollect mobile data collection application was used daily to collect data on the number of samples collated per testing site. Cases were investigated using the paper-based case investigation form and data was entered into the Surveillance Outbreak Response Management and Analysis System (SORMAS) national database. Key data elements collected using the ODK form include the socio-demographic characteristics, symptoms, hospitalization and travel history, and epidemiological details.
A centralized approach to contact tracing was being implemented in the state prior to this intervention. The LGA DSNOs were saddled with the responsibility of tracing and monitoring contacts of confirmed cases. However, they were often overwhelmed with activities due to inadequate staff at the LGAs and other competing activities. Following discussions with the Nigeria Red Cross Society (NRCS) Ondo State branch, the organization volunteered to support contact tracing activities, leveraging on their existing pool of community volunteers at the wards and divisional supervisors at the LGAs. One volunteer per ward (a total of 34) and one divisional supervisor per hotspot LGA were trained on home-based care monitoring and contact tracing. The volunteers and NRCS divisional supervisors conducted contact tracing, including identification of contacts for line-listing and follow-up for 14-days. The LGA DSNO who has access to details of new confirmed cases using the SORMAS database ensured that the details were communicated timely with the NRCS divisional supervisors who in turn shared with the volunteers in the communities. The volunteers ensured enrollment of confirmed cases who had mild or no symptom into HBC monitoring and followed them up for 14-days. Details of patients on HBC monitoring and contacts line-listed and followed-up were collected using the KoboCollect data tool, which was used to transmit data timely to the LGA and state case manager who already had access to the platform to coordinate activities in the communities.
The following variables were included in the contacts line-listing and monitoring forms: socio-demographic characteristics (name, age, sex, occupation), type of contact with case, symptoms and outcomes (alive, transferred, death, defaulter and discharged). The community volunteers were expected to send the forms daily and share weekly reports with the divisional supervisors, who shared contact tracing reports with the LGA DSNO, HBC monitoring data with the LGA home based-care supervisor. The LGA DSNOs and case managers communicated these reports with the State PHEOC pillar heads.
Prior to the intervention, the state-level EOC meeting was held weekly up to February 2021, while no LGA EOC meeting had been held in any LGA. The state epidemiologist coordinated virtual EOC meetings with members of the EOC pillars and partners at the state level, however, there was constant interruptions particularly during active discussions as the free virtual calls ended after 40 minutes. Moreover, members of the PHEOC were often unable to connect regularly to the meeting link due to the lack of data bundles to sustain lengthy discussions during meetings. These circumstances have resulted in the cessation of EOC meetings in the state. Following WHO support for subscription and data refunds for the EOC, the meetings were held regularly and seamlessly. The state EOC pillar heads were also supported to analyse data and make presentations during the meetings.
At the LGA level, there had not been an organized set up of EOC since the commencement of the pandemic in 2020. Thus, guidance on the set up of EOC members at the LGAs was provided accordingly based on national guidelines, which included a minimum of 6 members: PHC coordinator, DSNO, LGA public health nursing officer or IPC and case management focal person, risk communicator/health education, laboratory technician and local government immunization officer/cold chain officer. The state and LGA RRT were provided with orientation on their roles and responsibilities during an enlarged virtual EOC. State supervisors were also deployed to support the LGAs, ensuring meetings were held regularly, with attendance and minutes of meetings taken, as well as deliberation of pillar reports and action points taken.
Case-based data were extracted from the state COVID-19 line-list from 3rd April 2020 to 22nd August, 2021 to review the overall epidemic situation of the outbreak. Also, three months of data prior (23 February to 23rd May, 2021) and three months during the intervention (24th May to 22nd August, 2021- Epi weeks 21 to 33) were analysed to show comparison between the number of cases and contacts reported. Data on number of EOC meetings held was verified using the meetings’ attendance sheets. The weekly case reports were analysed to show trends of cases tested and test positivity rate (TPR). Data were imported into SPSS version 25 and analyzed. Descriptive analysis such as charts and maps were used to show the overall epidemic situation, prior and during the period of intervention
A total of 31,286 suspected cases were investigated and tested for COVID-19 between 23rd February to 22nd August 2021, of which 3,927 cases were confirmed with case fatality ratio (CFR) of 1.8%. Among the 18 LGAs in the state, Akure South had the highest confirmed cases of 1990 (50.7%) followed by Owo LGA (542; 13.8%). The majority (n=3,139, 79.9%) of the cases were between 20 – 59 years of age, with mean age of 38.5±18.1. Slightly above half (n=2119, 54.0%) of the cases were males (Table 1). A high proportion (n=553, 61.9%) had tertiary level of education, followed by secondary (n=2865, 73.0%).
Table 1
Characteristics of confirmed cases in Ondo State and the three hot spot LGAs
| Variable | State n (%) N=3,927 |
Akure South, Akure North and Owo LGAs n (%) N=2878 |
|---|---|---|
| LGA | ||
| Akure South | 1990 (50.7) | |
| Owo | 542 (13.8) | |
| Akure North | 346 (8.8) | |
| Ondo West | 297 (7.6) | |
| Okitipupa | 270 (6.9) | |
| Akoko North East | 239 (6.1) | |
| Ose | 36 (0.9) | |
| Other LGAs* | 207 (5.2) | |
| Age | ||
| <5 | 66 (1.7) | 50 (1.7) |
| 5-19 | 263 (6.7) | 236 (8.2) |
| 20-39 | 1868 (47.5) | 1259 (43.7) |
| 40-59 | 1271 (32.4) | 987 (34.3) |
| ≥60 | 459 (11.7) | 346 (12.1) |
| Gender | ||
| Female | 1808 (46.0) | 1397 (48.5) |
| Male | 2119 (54.0) | 1481 (51.5) |
| Level of education completed | ||
| None | 51 (1.3) | 46 (1.6) |
| Nursery | 18 (0.5) | 14 (0.5) |
| Primary | 203 (5.2) | 167 (5.8) |
| Secondary | 790 (20.0) | 466 (16.2) |
| Tertiary | 2865 (73.0) | 2185 (75.9) |
| Outcome of case | ||
| Recovered | 3764 (95.8) | 2772 (96.3) |
| Yet to recovered | 93 (2.4) | 58 (2.0) |
| Died | 70 (1.8) | 48 (1.7) |
*Akoko South West, Akoko North West, Akoko South East, Idanre, Ifedore, Ondo East, Irele, Ese Odo, Ilaje, Ile-Oluji/Okeigbo, and Odigbo
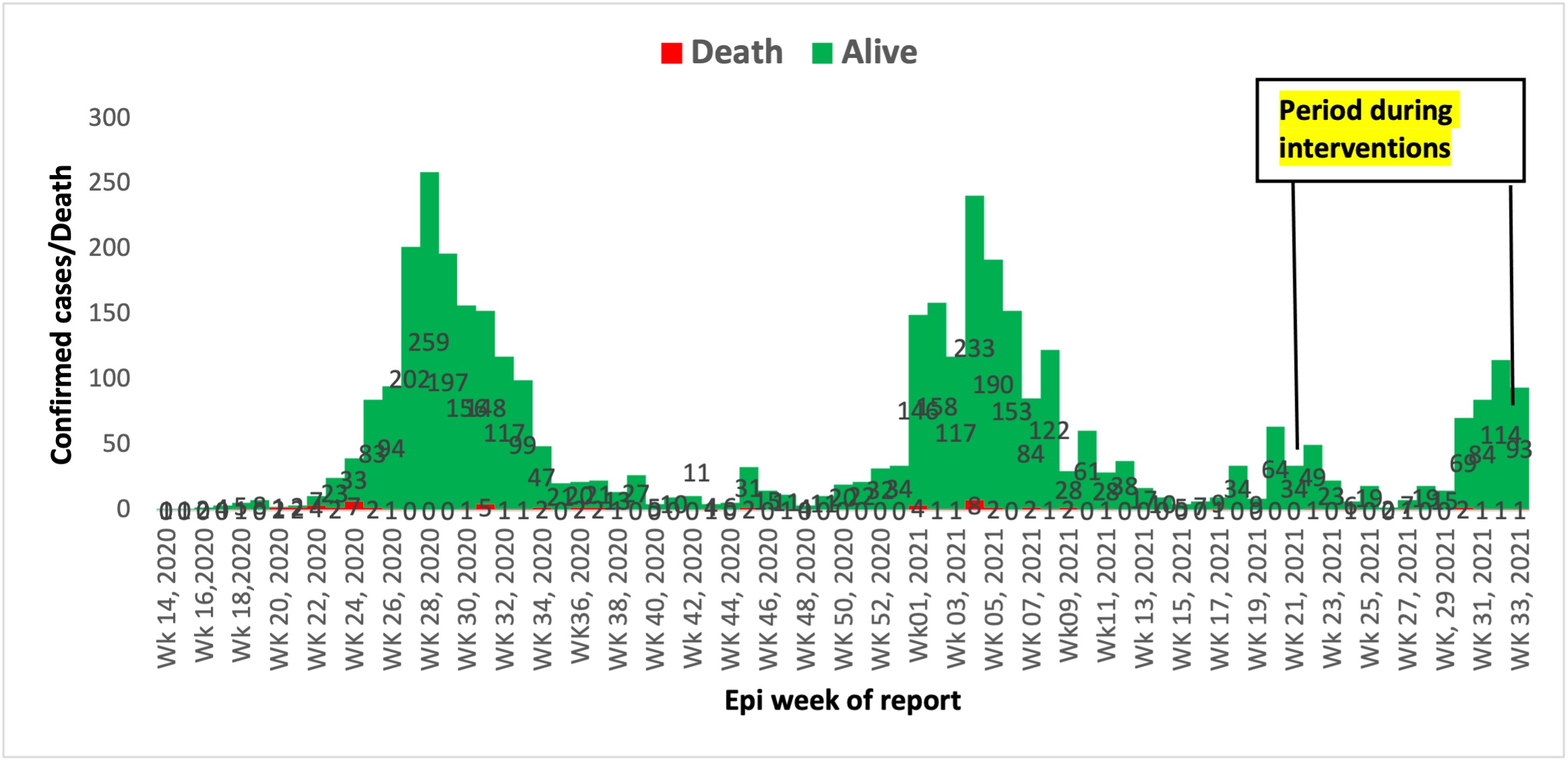
Figure 1 shows the epidemic curve of the outbreak from epi-week 14 (3rd April), 2020 to epi-week 33 (22nd August), 2021. The curve shows four waves of the COVID-19 outbreak since the report of the index case on April 3, 2020, with peak of cases on 12 July during epi-week 28 of 2020 (259 cases), 31 January 2021 (233 cases), 23 May 2021 (64 cases) and 12 September 2021 (114 cases) respectively.
Weekly Epi-Curve of COVID-19 cases and deaths in Ondo State, April 2020 to August, 2021
Generally, 3880 suspected cases were tested and 456 cases were confirmed for COVID-19 during 3 months of integration of sample collection into healthcare services at the facility level in the three hotspot LGAs compared to 1668 samples tested and 204 cases confirmed in three months before the intervention. Specifically, 1451 (During: 1318 vs before: 133) samples were tested in Akure North, 2467 (During:1428 vs before: 1039) in Akure South and 1630 (during 1134 vs before: 496) in Owo LGA respectively (Figure 2). There was a reduction in test positivity rate in Akure North and Owo LGAs in the period during the intervention (Akure North; 10% and Owo; 9%) compared to the period prior to intervention (Akure North; 17% and Owo; 11%)
Comparison between COVID-19 samples tested in 3 months before and 3 months during intervention in 3 hot spot LGAs
Figure 3 shows the distribution maps of COVID-19 cases tested across the 34 wards in the three hot spot LGAs. All 34 wards in the three hotspot LGAs reported and tested suspected cases, with 35.3% of the wards having tested > 100 suspected cases during the period of intervention compared to the period before the intervention where 6 of the 34 (17.6%) wards have not reported a single case, and only 2 (5.9%) wards reported >100 suspected cases (as indicated with purple colour) (Figure 3).
Comparison between COVID-19 suspected cases by wards before and during intervention in 34 wards in the three hot spot LGAs, Ondo State
In Figure 4, the number of contacts traced and line-listed during the period of intervention compared to the period before intervention was lower for both Akure South (458 vs 795) and Owo LGAs (225 vs 297) respectively. However, slightly higher number of contacts were line listed during the intervention periods (95) compared to periods before intervention (78) in Akure North LGA. Generally, the case to contacts ratio dropped from 1:5 before intervention to 1:1 during the interventions in the three hot spot LGAs.
Comparison between contacts of COVID-19 cases line-listed in three months before and during intervention in three hot spot LGAs in Ondo State
It was found that there is 25% increase in the expected number of State EOC meetings held during the intervention period (11, 92.0%) compared to pre-intervention period (8, 67.0%). For LGA EOC meetings held in the three hot spot LGAs, 10 (83%) of the 12 expected meetings were held within the period of intervention compared to none held before the intervention period.
Overall, the highest proportion of COVID-19 cases tested were reported in Akure South, Akure North and Owo LGAs respectively since inception of the outbreak up to the intervention period of 22 August 2021. Thus, these LGAs with consistent report of cases were identified as hotspot areas, and considered for enhanced public health response or interventions. Similar to previous outbreak settings, a high proportion of cases were male and within the economically active age group of 20 to 59 years (12). This suggests high exposure to infection among men and younger age groups with greater potential roles in socio-economic activities than their counterpart. Furthermore, the epidemiological curve suggests a propagated pattern of transmission of infection, with four waves of outbreak observed, which indicates high person-to-person or community transmission. This pattern of outbreak was consistent with previous COVID-19 outbreak reports in Oyo State (12), Nigeria, across 35 States and Federal Capital Territory in Nigeria (13) and China (14). This finding suggests the need to intensify the use of the Public Health Social Measures (PHSM) such as the non-pharmaceutical individual and societal interventions to reduce transmission in the community.
Our findings suggest that integrating COVID-19 sample collection into routine health care services positively increased testing and reduced number of silent wards. This shows that integrating sample collection for COVID-19 into to the routine health care services is feasible. However, costs of transportation of specimens from health facilities to the nearest testing centre will have to be borne. Integrating rapid antigen testing into the health service in this manner will not require such additional costs. In this study, the implementation of COVID-19 sample collection for testing at health facility level may have contributed to the increase in number of cases reported across the wards during the intervention compared to earlier periods in the pandemic response. Similar to our finding, Church et al. (2017) used a different methodological approach of non-randomized cohort to assess the impact of integrated reproductive health and Human Immunodeficiency Virus (HIV) services comprising of a training and reorganization, and receipt of reproductive health and HIV services, on HIV testing and counseling among family planning clients, and found that it resulted in increased in HIV testing and counseling (HTC) in Kenya (15). In Kaduna State Nigeria, an integrated COVID-19 and tuberculosis (TB) case finding intervention was also successfully implemented using existing TB structure, with high proportion of patients screened for COVID-19, TB and HIV between June and July. 2020 (16).
Fewer contacts were line-listed during the period of intervention compared to the period before the intervention. The continued increase in the number of cases between June and August 2021 (period of intervention) may have overwhelmed the human resource or volunteers engaged to conduct the contact tracing activities, whereby, one volunteer per ward was conducting several activities, such as contact tracing, 14-days follow-up of contacts and home-based care monitoring of cases which are increasing and widely dispersed across the ward. This may also be attributed to delayed turn-around time of laboratory results, which may have led to disbelieve in the tests’ results among patients and their non-willingness to disclose contacts in the face of stigmatization. Similar to our findings, Ukwenya et al. (2021) found that more than one-third of community members in Ondo State, Nigeria were unwilling to disclose their contacts after testing positive for COVID-19 (17).
The functionality of the Public Health Emergency Operation Center (PHEOC) continues to be a major concern among member states of the WHO African Region (18). The EOC plays a critical role in supporting the Member States to prepare for and respond to public health emergencies to fulfill the International Health Regulations (IHR) Obligations. At the initial stage of the response in the state, coordination and implementation of all activities were done at the state level or centrally, with minimal LGA involvement in coordination of outbreak response. Following the interventions, LGA EOC meetings commenced in the 3 hotspot LGAs under the leadership of the Medical Officers of Health who oversee all outbreak response in the LGA. This may have contributed to the detection of more cases and accelerated response at these LGAs. We found that the state EOC meetings were conducted regularly during the period of intervention thus, enabling the state to use the existing state EOC structure to respond to other outbreaks such as Lassa fever and Cholera. Similar to this finding, decentralized response improved coordination at the district level in Lagos State, Nigeria (19).
Preliminary data on home-based care monitoring and contacts followed-up prior to the intervention could not be assessed or not available because there was no organized system for collecting such data before the intervention. Thus, comparison of such data could not be made in this study.
Strengthening decentralization of response including the commencement of local government area EOC meetings and integration of COVID-19 sample collection for testing to routine healthcare services positively influenced high number of cases tested and reported across the wards in the three hot spot LGAs. The fewer number of contacts traced and line-listed during the period of intervention despite engagement of community volunteers suggests the need to explore an alternative method of contact tracing such as digital contact tracing, through engaging cases to self-report contacts using an application on their smartphones to reduce stigma from visiting contact tracers or teams. In addition, there may be a need to intensify the engagement of community and religious leaders, and key community groups as integral members of the contact tracing team or volunteers, and in disseminating information on the importance of contact tracing to the community members. Furthermore, there is need to introduce the antigen detecting rapid diagnostic (Ag-RDT) test kits at health facilities in order to intensify testing and prevent additional costs that can result from samples transportation to the molecular PCR laboratory.
The intervention assessed form part of the State’s response to the COVID-19 pandemic, and thus it was regarded as a non-research program evaluation. It required no direct contact with human subjects and only used identified pooled data collected routinely during the outbreak.
The authors declare that they have no competing interests.
Authors AMA and AAF conceived the study, conducted the analysis and wrote the first draft of the manuscript. All authors reviewed the first draft and approved the final manuscript.
We acknowledge the efforts of the State and LGA personnel who responded tirelessly to the outbreak.
1. Center for Disease Control. Novel Coronavirus, Wuhan, China. Available at: https://www.cdc.gov/coronavirus/2019-nCoV/summary.html. Accessed 02/02/2022.
2. World Health Organization. Weekly Operational Update on COVID-19—18 MAY 2022. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20220518_weekly_epi_update_92.pdf?sfvrsn=fca4e67f_4&download=true. Accessed 24/09/ 2021.
3. Africa CDC. Available at: https://africacdc.org/download/outbreak-brief-88-coronavirus-disease-2019-covid-19-pandemic/?ind=1632251993471&filename=AfricaCDC_COVIDBrief_21Sep21_EN.pdf&wpdmdl=9979&refresh=614e3a50d72311632516688. Accessed 02/12/2021
4. NCDC. COVID-19 Nigeria. Available at: https://covid19.ncdc.gov.ng/. Accessed on 19/10/2021.
5. NCDC. COVID-19 Situation report. Weekly Epidemiological Report 46, Epi week 34: 23rd – 29th August, 2021. Available at: https://ncdc.gov.ng/themes/common/files/sitreps/64fc9fdf692648120a5d93651d136c14.pdf. Last accessed 05/02/2022.
6. Dan-Nwafor C., Lucia Ochu C., Elimian K., Oladejo J., Ilori E., Umeokonkwo C., Steinhardt C. et al.. Nigeria’s public health response to the COVID-19 pandemic: January to May 2020. View Points. 10 (2): 020399. doi: 10.7189/jogh.10.020399.
7. Ajisegiri WS, Odusanya OO & Joshi R. COVID-19 Outbreak Situation in Nigeria and the Need for Effective Engagement of Community Health Workers for Epidemic Response, Global security 2020; 1(4).
8. NCDC. Government laboratories. Available at: https://covid19.ncdc.gov.ng/laboratory/. Accessed 17/10/2021.
9. National Bureau of Statistics (2020) 2017 Demographic Statistics Bulletin. https://nigerianstat.gov.ng/download/474.
10. Shuaib F, Gunnala R, Musa EO, Mahoney FJ, Oguntimehin O, Nguku PM, et al. Ebola virus disease outbreak- Nigeria, July-September 2014. MMWR 2014; 63(39): 867-72.
11. WHO. Coronavirus disease 2019 (COVID-19) Situation Report- 72, 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200401-sitrep-72-covid-19.pdf. Accessed 25/05/2022.
12. Usman, A.B., Ayinde, O., Akinyode, A., Gbolahan, A. and Bello, B. Epidemiology of Coronavirus Disease 2019 (COVD-19) Outbreak Cases in Oyo State South West Nigeria, March-April 2020. Pan Afri. Med J, 23;35 (Suppl): 88. Available at: https://doi.org/10.11604/pamj.supp.2020.35.2.23832. doi: 10.11604/pamj.supp.2020.35.2.23832
13. Elimian, K.O., Ochu, C.L., Ilori, E., Oladejo, J., Igumbor E., Steinhardt, L., et al. Descriptive Epidemiology of Coronavirus Disease 2019 in Nigeria, 27 February- 6 June 2020. Epidemiol Infect., 148, e208: 1-16. https://doi.org/10.1017/S095026882000206X
14. Chen, T., Guo, S. and Zhong, P. Epidemic Characteristics of the COVID-19 Outbreak in Tianjin, a Well-Developed City in China. Am J Infect Control, 2020. 48 (9): 1068-73. https://doi.org/10.1016/j.ajic.2020.06.006.
15. Church K., Warren C.E., Birdthistle I., Ploubidis G.B, Tomlin K., Zhou W., et al. Impact of Integrated Services on HIV Testing: A Nonrandomized Trial among Kenyan Family Planning Clients. Stud Fam Plann, 2017. 48(2): 201- 18.
16. Gidado M, Odume B, Ogbudebe C, Useni S, Tukur M, Chukwuogo O, et al.. Early experience in implementation of an integrated COVID-19 and TB community-based active case finding. African J Respir Med, 2020. 15 (2): 18-23.
17. Ukwenya VO, Fuwape TA, Ilesanmi OS and Afolabi AA. Willingness to participate in testing, contact tracing, and taking the COVID-19 vaccine among community members in a Southwestern state in Nigeria. Global Biosecurity, 2021; 3(1).
18. WHO Regional Office for Africa. Handbook for Public Health Emergency Operations Center Operations and Management Brazzaville:. Licence: CC BY-NC-SA 3.0 IGO. Available at; https://africacdc.org/download/handbook-for-public-health-emergency-operations-center-operations-and-management/#. Accessed 19th October, 2021.
19. Mueller UE., Omosehin O., Akinkunmi AE., Ayanbadejo JO., Somefun EO., Momah-Haruna. Contact Tracing in an African Megacity during COVID 19: Lessons Learned. Afr J Reprod Health, 2020 (Special Edition on COVID-19); 24 (2):27. DOI: 10.29063/ajrh2020/v24i2s.4.